Page 1
Ninth Circuit:
Putative Class Action Against Rite Aid Won’t Be Arbitrated
Smith Says Allegations of Harm to Consumers in Form of Hiked Co-Payments—Through Allegedly Inflating Prices to Insurers—Doesn’t Implicate Arbitration Clauses in Contracts With Insurance Companies’ Intermediaries
By a MetNews Staff Writer
A putative class action against Rite Aid for allegedly inflating its prices in billing intermediaries of insurance companies, meaning higher co-payment prices, will not be re-routed to arbitration, under a decision Friday by the Ninth U.S. Circuit Court of Appeals.
Rite Aid insisted that the action brought by a consumer, Bryon Stafford, is subject to arbitration based on provisions in its contracts with the intermediaries, pharmacy benefit managers (“PBMs”) and third-party payors (“TPPs”). Under the doctrine of equitable estoppel, a plaintiff whose claims rely on contracts between others is bound by the provisions of those instruments.
Circuit Judge Milan D. Smith Jr. wrote for a three-judge panel in declaring that the doctrine does not apply to the action brought by Stafford, affirming an order by District Court Judge Anthony J. Battaglia of the Southern District of California (now a senior judge) denying Rite-Aid’s motion to compel arbitration.
|
|
|
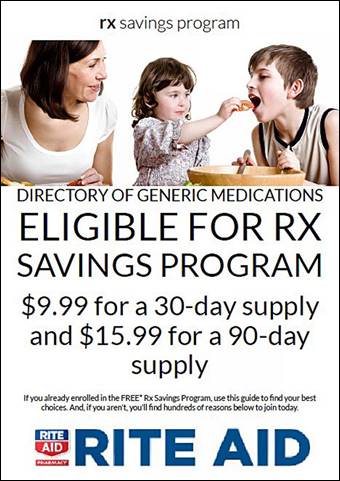
Rite Aid offers customers without health insurance cost-breaks on generic drugs, as reflected by ad above. Two putative class actions allege that Rite Aid charges higher prices to insurance companies, despite an obligation to charge “usual and customary” prices, and that the inflated prices mean that customers with insurance plans are charged excessive co-payments. The Ninth U.S. Circuit Court of Appeals on Friday held that the action is not to subject arbitration clauses in Rite Aid’s contracts with the insurers’ intermediaries. |
Allegations of Complaint
The operative complaint, at the time of Battaglia’s ruling, set forth sets forth:
“At bottom, this action concerns Rite Aid’s illegal practice of overcharging customers enrolled in public or private health care plans for generic prescription drugs by submitting to third-party payors claims for payment at prices that Rite Aid has knowingly and intentionally inflated above its ‘usual and customary’ prices. As a result, customers who purchase generic prescription drugs through third-party plans pay copayments that are significantly more than Rite Aid’s ‘usual and customary’ prices for those same drugs.”
The pleading continues:
“The lynchpin of Rite Aid’s scheme is its Rx Savings Program (‘RSP’), a prescription savings program that allows cash-paying customers—those who pay for drugs without using insurance—to purchase 350 of the most commonly prescribed generic drugs listed on Rite Aid’s special formulary…at price levels, generally, of only $9.99 for a thirty-day supply and $15.99 for a ninety-day supply…The RSP Prices, however, are often significantly lower than the prices that Rite Aid reports to health insurance companies as Rite Aid’s ‘usual and customary’ prices, and thus, the amounts that individuals using insurance must pay for the dings in the form of a copayment.”
Battaglia’s Ruling
In denying Rite-Aid’s motion, Battaglia said:
“There is no doubt that there is some relation between Plaintiff s claims and the contracts between Rite Aid and the TPP/PBMs. But the pertinent question is whether Plaintiffs claims are ‘dependent upon, or inextricably intertwined’ with Rite Aid’s contractual obligations to the TPP/PBMs….[T]he answer to that question is no. Plaintiffs claims do not necessarily depend upon the contracts between Rite Aid and the TPP/PBMs.”
He said the action is based on an alleged fraudulent scheme under which the intermediaries are over-charged resulting in higher co-payments being charged customers with health plans.
“That this litigation might involve reference to the contracts between Rite Aid and the TPP/PBMs is not enough to find dependence or inextricable intertwinement with the contracts,” he wrote.
Smith agreed. He wrote:
“It is irrelevant whether the contracts between Rite Aid and the pharmacy benefits managers required Rite Aid to report the usual and customary price of a prescription drug. Even if the contracts contained no provision requiring Rite Aid to report the usual and customary price, the fact remains that Rite Aid did report that information and allegedly purposely inflated it. Rite Aid’s duty not to commit fraud is independent from any contractual requirements with the pharmacy benefit managers….[S]tatutes and common law—not provisions in the contracts—entitle Stafford to relief. The principles of equitable estoppel therefore do not require Stafford to submit to the arbitration clauses of contracts between Rite Aid and the pharmacy benefits managers.”
The case is Stafford v. Rite Aid Corporation, 20-55333.
Stafford has pled claims under California’s Unfair Competition law and Consumer Legal Remedies Act, as well as for unjust enrichment and negligent misrepresentation. His action was consolidated for trial with a similar one brought by Robert Josten.
Subsequent to Battaglia’s Feb 24, 2020 ruling denying the motion to compel arbitration of Stafford’s action, each amended his complaint.
Proceedings in the cases were stayed pending appeal on July 30, 2020. On Oct. 6 of that year, the cases were shifted to District Court Judge Todd Robinson.
Copyright 2021, Metropolitan News Company